Jumper’s Knee: How is it different from Runner’s Knee?
(..and what to do about it.)
Runner’s knee was discussed in the previous article detailing a pain that is felt around the knee cap, caused by altered biomechanics, mostly at the hip.
In jumper’s knee, also known as patellar tendinopathy (PT), the pain is located on the front of the knee. One can easily pinpoint it when asked to show where the pain is, in contrast to Runner’s knee. Exactly beneath the knee cap and between the shin bone (tibia), is a thick tendon called the patellar tendon. The tendon will usually ache in the morning or at the start of an activity, with the pain returning after activity when you have cooled down. If left untreated and the condition allowed to progress, it will become constantly painful and also limit function. The tendon might also feel thickened when compared to the other side. The exact mechanism of injury is still not known but considering the anatomical position of the patellar tendon, it has to be able to compress, stretch and recoil depending on the forces applied.
Van Ark et al. (2016) defined the injury mechanism as a repetitive, excessive overload injury to the extensor mechanism of the knee. It is most common in sports with a lot of explosive jumping such as volleyball or basketball but is also found in approximately 5% of all running injuries as revealed by Tauton in 2002.
A systematic review by Morgan et al. (2016) identified risk factors that predispose an athlete to this type of injury:
- Reduced quadriceps strength.
- Inappropriate training load progression/duration.
- Reduced flexibility (especially Quadriceps and Hamstrings).
- Poor running mechanics (Consider appropriate running shoes too).
- Inferiorly displaced patella.
What can be done to avoid this problem?
In my experience, the most important factor when starting a running program is to listen to your body. It is normal to feel aches and pains after training, especially if your body is still getting used to the new stresses that you are subjecting it to. When pain becomes a constant in your life it is best to have it checked out by a professional in the field to avoid it becoming a chronic overuse injury. Load management is key and a tailored and progressive program will allow your body to adjust without causing damage to your tendons.
What can be done to treat it?
There are several treatments on offer that claim miraculous benefits and immediate effects. Unfortunately, in my opinion, these alone will not work without a properly tailored and graded exercise protocol. Tendinopathies will only heal if they are loaded correctly!
Several exercise regimens and varieties have been studied but the most effective fall into 3 categories:
- Isometrics (Where muscle contracts but remains at the same length).
- Eccentrics (Where muscle contracts but lengthens at the same time).
- Heavy slow resistance (HSR).
A systematic review by Lim and Wong (2017) has found that isometrics are the safest to use, but no studies confirm that they actually work in the long term. Eccentric protocols are effective in most clinical situations but are difficult to pursue within an active racing season and would entail difficult integration into the athlete’s training routine. HSR should be applied carefully and tailored to the unique circumstances of each athlete.
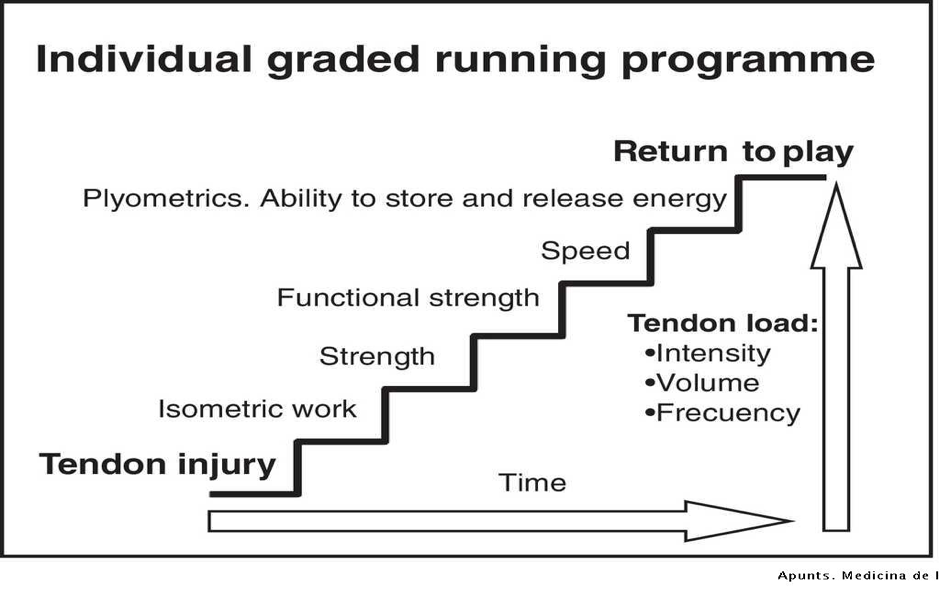
There is no recipe that applies to everyone. An intelligent and critical approach must be taken to ensure a proper return to full function and not just the elimination of symptoms. The figure below by Mascaro et al. (2018) tries to explain that rehabilitation following tendinopathy is an intelligent stepped approach that entails a clever tweaking of intensity, volume, and frequency of training.
In my opinion, when faced with a PT, correct loading of the aggravated tendons is the only way forward. Everything else is helpful to control pain but not to actually tackle the solution.
Look for help from an experienced physiotherapist and make sure that you commit to the program without missing any of the steps!
Simon Cilia